Telemedicine app development: How to build a doctor on demand app

Telemedicine has attracted lots of interest from clinics, doctors, and patients. In 2023, the global telemedicine market was valued at $114.98 billion and is expected to grow at a CAGR of 18.6% reaching $380,33 billion in 2030, according to the Grand View Research.
We’re going to talk about how remote care can address problems of access, quality, and cost in delivering healthcare services. We’ll also give an overview of the telemedicine market and share the ins and outs of doctor on demand app development.
What is a telehealth app and what problems does it solve?
A telemedicine app lets patients consult with doctors remotely. Take MDLIVE as an example. This telehealth mobile app works 24/7, letting patients choose doctors and talk to them by phone or video. Another great example is Amwell, a healthcare app that allows users to choose a doctor and have a video visit with them. Doctors can then send prescriptions right to the patient’s pharmacy.

Source: dribbble.com by Brian Turley
Why is telemedicine so important? Because it fills the gaps in healthcare.
1. Barriers to health services in rural and remote areas
People living in rural and remote areas experience poor access to a variety of medical services. According to a report on non-urgent emergency visits in rural and urban areas by the Maine Rural Health Research Center, rural residents face more barriers to accessing care such as fewer physicians per capita, greater difficulty to after-hours care, and higher uninsured rates compared with urban residents. With telemedicine, rural patients don’t need to travel long distances to access health care, instead having virtual visits with doctors.
2. Limited access to healthcare for elderly and disabled patients
Elderly patients and those with disabilities may have difficulties accessing hospitals. With telemedicine, anyone can access care from the comfort of their home. All patients need to do is choose a healthcare provider and book an appointment for a suitable time.
3. Problems with patient monitoring
If integrated with an EMR (electronic medical records) system, a telemedicine app offers healthcare providers real-time access to patients’ health data. Thanks to this, doctors can monitor patients on the go and provide advice when health indicators worsen. This is particularly important for patients with chronic diseases.
4. Long waits for appointments and long travel times
Patients no longer have to travel long distances to access medical care and wait at a doctor’s office. With telehealth technologies, patients can meet with a doctor right away or schedule an appointment for a precise time.
Telemedicine in 2024
Before we go into detail about must-have features of a doctor-on-demand app, let’s look at the telemedicine market to understand what attracts patients and doctors to telehealth technologies and see the current state of virtual care.
What is the current state of eHealth?
According to IMARC Group, the global telehealth market was valued at $141 billion in 2024 and is expected to grow to $538.9 billion by 2033. There are quite a lot of factors that drive the growth of telehealth services including:
- Evolving patient needs
- Medical staff shortage and the growing need for healthcare services
- Advancements in technology like artificial intelligence (AI), machine learning (ML), and data analytics (DA)
- Rising investments in the healthcare IT infrastructure
- Growing demand for remote healthcare services
- High cost of traditional care
- Positive experiences of early adopters
Some more interesting statistics provided by Precedence Research:
- In 2023, North America dominated the global telehealth market with a market share of 54%. Yet Asia Pacific is expected to be the most opportunistic market during 2024-2034.
- By product type, the services segment accounted for the largest revenue share in 2023. However, the software segment is expected to be the fastest-growing segment during the forecast period (2024-2034).
- By end user, the hospitals segment dominated the global telehealth market with a revenue share of 57%. This segment is anticipated to continue its dominance during 2024-2034.
- By platform, web-based solutions were preferred, having a market share of 48.5% in 2023.
What do patients say about telemedicine?
A report by Statista says that there were more than 116 million users of doctor appointment apps globally in 2024, compared to 57 million in 2019. The telemedicine adoption will continue to grow since it has been well-received not only by doctors but also patients.
As of March 2021, 86% of patients in the US said healthcare has become more accessible due to telemedicine while 63% of patients reported that their fear of doctors or medical procedures were eased with telemedicine. Another contributing factor to telemedicine patient adoption was reported to be time and cost savings.
Another report says that more than half of patients surveyed in the US expressed better satisfaction with their care owing to telemedicine in 2023. And only one in ten respondents indicated lower patient experience and satisfaction.
What do physicians say about telemedicine?
Physicians who have used telehealth say they have seen:
- better patient access to healthcare (93%)
- increased productivity (77%)
- cost reductions (71%)
- better patient-doctor communication (71%)
- improved relationships with patients (60%)
According to the AMA digital health care 2022 study, the percentage of physicians using telehealth or virtual visits increased from 14% in 2016 to 80% in 2022, and the number of physicians using remote monitoring devices grew from 12% in 2016 to 30% in 2022. What's more, there has been a boost in the percentage of physicians who see significant benefits in leveraging digital health solutions, from 85% in 2016 to 93% in 2022.
Among the major reasons why physicians are willing to use direct-to-consumer (DTC) telemedicine are to:
- improve patient access to healthcare services
- have a better work-life balance
- attract and retain patients
- improve patient outcomes
- be at the forefront of medicine
Statistics show that nowadays only about 8% of physicians see no advantage or some disadvantages in the adoption of digital tools. Let's see what can be the top barriers and areas of doubt for these 8%.
What are the biggest barriers to telemedicine?
Among the top barriers to telehealth are:
- Uncertainty about reimbursement. To address this concern, the US Centers for Medicare and Medicaid Services (CMS) have suggested that Medicare Advantage plans cover telemedicine services. Additionally, 48 states provide doctors with reimbursement for telemedicine services via the Medicaid fee-for-service model. Lots of states also require insurers to provide telehealth.
- Clinical appropriateness. Some doctors are worried that clinics aren’t equipped for telemedicine. Therefore, some medical establishments take actions to ensure clinical quality is upheld during telehealth visits. Take the Cleveland Clinic as an example. They reviewed the quality of virtual visits, developed templates so physicians can fully document their virtual visits, and established guidelines on antibiotic appropriateness to ensure that quality standards are maintained when providing remote care.
- Concerns about quality of care. Medical practices need to ensure that healthcare quality is maintained throughout telehealth visits.
- Poor buy-in. Some doctors believe telemedicine visits will replace face-to-face visits and will provide poor quality of health services. Avera Health, a regional health system in South Dakota, deals with doctors’ resistance to adopting telemedicine through informative write-ups and in-person meetings.
- Lack of support from hospital leadership. Leaders can contribute to successful telehealth adoption by physicians. When leaders show support, physicians are motivated and are quicker to adopt telemedicine visits. American Well saw this problem and started working with clinical leadership to develop strong support for telemedicine services.
The COVID-19 situation led to a larger spike in telemedicine adoption. Below are some interesting statistics to prove this:
- In 2020, 48% of physicians used telemedicine solutions to treat patients (Source: Merritt Hawkins), up from 18% in 2018. (Source: The Physicians Foundation)
- Fifty-two percent of doctors are planning to use telemedicine more. (Source: The Physicians Foundation)
- In March 2020, seventy-six percent of patients were interested in using telemedicine, compared to 11% in 2019. (Source: McKinsey & Company)
- Fifty-seven percent of doctors view telemedicine more favorably than they did before the coronavirus outbreak, while 64% are more comfortable using it. (Source: McKinsey & Company)
- About 100, 000 physicians (12% of respondents) have moved to a primarily telemedicine position. (Source: The Physicians Foundation)
- To expand reimbursement for telemedicine services to Medicare beneficiaries, the Centers for Medicare & Medicaid Services (CMS) now allows for over 80 new services to be furnished via telemedicine. (Source: CMS.gov)
- During COVID-19, American Well went public and its shares soared over 28% in the first day of trading. (Source: Barron’s)
Features to include in your telemedicine app
To better understand what features to include in your virtual visit app, let’s take a look at a typical user journey in a telemedicine app.

Source: Globaldev
Apps differ, and so do their user journeys. For example, the user journey in the Doctor On Demand app is a bit different from the one we’ve just described. Here’s how a user interacts with Doctor On Demand:
- Lists symptoms
- Shares their medical history
- Starts a visit
- Shows symptoms to the doctor using their phone’s or iPad’s camera
- Gets a prescription
Now that we know how a patient navigates a telemedicine app, we can outline the main features of an app for patients.

What about an app for doctors?
As for the doctor app, the user journey looks like this:
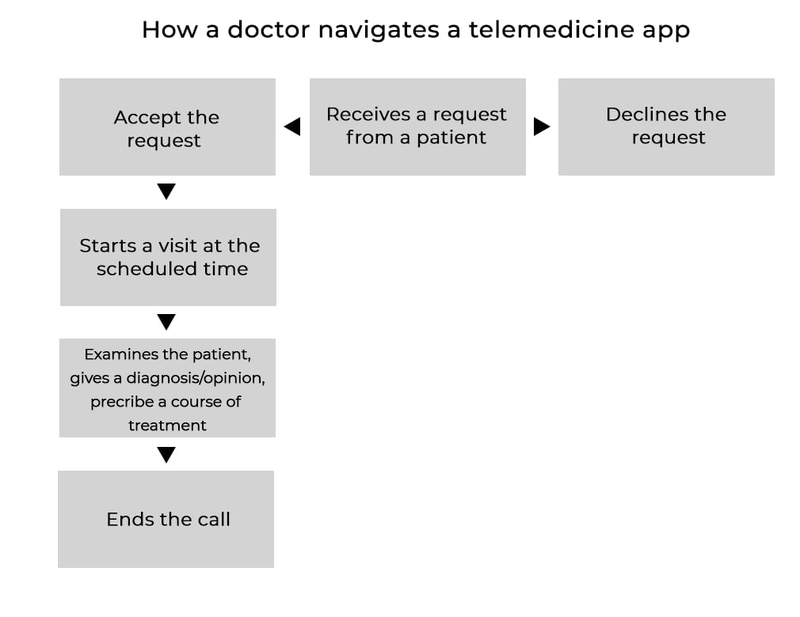
Source: Globaldev
Based on the user journey we’ve just outlined, let’s highlight the main features of a telemedicine app for doctors.

Top telehealth mobile apps
Where can you get ideas and inspiration for your doctor on demand app? From the top telehealth apps, of course. We browsed the top telemedicine apps and singled out the three most interesting.
Doctor On Demand
Doctor On Demand is a telemedicine app that’s available in the App Store and on Google Play. This app offers services such as urgent care, behavioral health, preventive care, and chronic care. With Doctor On Demand, patients can connect with board-certified doctors via video, list symptoms, share medical histories, get prescriptions, and share Apple HealthKit data with care providers (using the iOS app).

Source: App Store
Direct Health
iOS for patients | iOS for doctors | Android for patients | Android for doctors
Direct Health is a HIPAA-compliant app that enables doctors and patients to connect. With Direct Health, patients can have virtual visits with doctors, veterinarians, and therapists through audio, video, or text chats, receive lab results, referrals, and prescriptions, invite doctors to the app, share HealthKit records with providers, and participate in group chats with doctors. Doctors can prescribe medicine, set rates and get paid, manage schedules, chat with peers, create group chats, and keep track of earnings.

Source: App Store
MDLIVE
MDLIVE is a US-based telemedicine company founded in 2006. The MDLIVE app connects patients with doctors through phone, tablet, and PC and offers help with over 50 routine conditions including allergies, colds, fever, cough, and respiratory problems. MDLIVE also provides virtual consultations with psychiatrists and dermatologists. When clinically appropriate, MDLIVE sends a prescription to the nearest pharmacy.
The app charges patients for every consultation:
- $0-82 for urgent care visits (can be less depending on the insurance plan)
- $0 for primary care
- $0-108 for talk therapy
- $0-284 for a psychiatry appointments
- $0-95 for a dermatology appointment
MDLIVE states that pricing depends on insurance, so copays for participating plans may be as low as $0. And since pricing is always shown upfront, you won't be met with a surprise bill.
How to monetize a doctor-on-demand app?
There are different ways to make money from health apps. In March 2024, the three most popular monetization strategies in the US included ads, in-app purchases, and subscriptions according to Statista. Advertising has become the preferred mobile monetization practice globally, making up the largest share of the app market revenues. One-third of apps decided to use ads in their products and only one-tenth decided to go with in-app purchases.
Speaking specifically about how healthcare apps are monetized, Research2Guidance outlines the following business models for digital healthcare solutions based on survey answers:
- Digital health service sales (40%)
- Medical/ connected device sales (32%)
- Tech licensing (32%)
- Bundle sales, like device plus apps (31%)
- Project-related service sales (28%)
- Data sales (21%)
- Medication sales (21%)
- In-app purchases (18%)
- Research and development service sales (10%)
- In-app advertisement (10%)
- Paid downloads (5%)
There are several popular monetization models among established apps:
- Membership ― Users pay a monthly or yearly fee to use the app. Myca Nutrition uses this model.
- Transaction fee ― The app charges patients a service fee for every visit, or charges on a per-minute basis. This is what Pakistan-based TeleDoctor by Telenor Group does. The platform charges patients $0.08 for each minute. Doctor On Demand, on the other hand, charges patients a 25% fee for every consultation.
- Software as a service ― License the app to private practices. The best examples of this model are American Well and Doctor On Demand. The latter charges hospitals nearly $1 a month for each employee.
How much does it cost to develop a telemedicine app?
How much does a doctor on demand app cost? This is a difficult question to answer. There are multiple factors that influence the cost of app development, from features to design to agency rates. But we aren’t here to leave you in the dark, so we’ll give you an example of a telemedicine project we built and show you how long it took us to develop.
One of our recent telemedicine projects for the Malaysian market enables doctor–patient communication using mobile devices. Before starting development, we researched target users and found that Malaysian physicians prefer tablets to smartphones, as tablets allow doctors to better see patients during video calls, view scans, and type. Therefore, we created two native iOS apps: one for doctors, who use iPads, and another for patients, who use iPhones.
The app for patients features:
- Symptoms list
- The ability to follow doctors
- Virtual visits through messages, audio, and video
- The ability to upload clinical information such as medical reports, CT and MRI scans, X-rays, and immunization records
- Payment functionality
- E-prescriptions and medication ordering
- Blog
The doctor app, on the other hand, allows doctors to store patient health records, manage schedules, and get paid for appointments.

Source: Globaldev
In total, this project took us 2,246 hours to build:
- UX: 170 hours
- UI: 207 hours
- Backend: 810 hours
- iOS: 895 hours
- Quality assurance: 98 hours
- DevOps: 66 hours
Interested in doctor on demand app development?
If you have an idea for a healthcare mobile app startup and are looking for a development partner, we’d be happy to help. Jot down your details and message below, and let’s connect!